Smart spending on healthcare
07.08.14
Many commentators are asking whether society can continue to support innovation in a way that publicly funded health systems can afford. My very clear view – based on all the evidence we have today – is yes.
The problem is straightforward. Bringing a medicine to market – from the lab to the patient – has not become any cheaper. If anything, the opposite is true with development costs rising almost exponentially in recent decades. At the same time, the size of the market on which private sector companies are able to recoup their costs has become much smaller – a natural result of increasing personalisation and specialisation of treatment, that is likely to continue in future. So does the fact that it’s more expensive to produce medicines for fewer people necessarily mean that medicines are (or will be) unaffordable for healthcare systems? Not necessarily.
When it comes to medicines, a key success factor for health care systems will be to ensure ‘rational use’. Where it is possible to treat a patient to target on an older cheaper medicine it should be done. But if a patient needs a more modern treatment, access should be provided at reasonable prices that reflect both the added value and the volume across the market – with low volume treatments naturally commanding a higher price. Getting this balance right ensures that everyone wins. Existing evidence shows clearly that countries actively managing rational use have lower spending growth for medicines as a whole – and therefore more potential ‘headroom for innovation’.
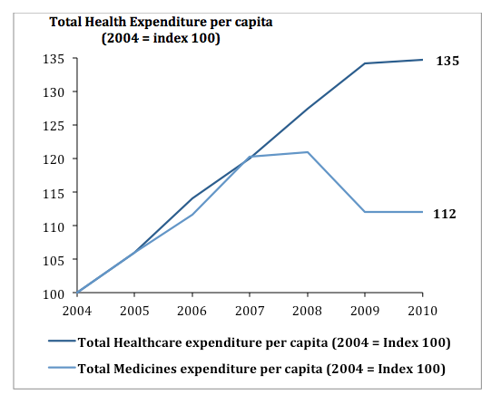
Across the OECD, medicines expenditure growth lags that of overall healthcare spending. The reason for this is that, despite the growth coming from new products, the off-setting savings derived from the loss of exclusivity of several major older products lead to reductions in price and, hence, savings that can be redeployed.
All this is not to say that we don’t have a challenge. Savings that accrue to one part of a health system often don’t get efficiently redeployed to where costs are rising. But it is an important message that the challenge of making health systems sustainable is not simply a debate about price or cost, it’s also about how resources get allocated – and about how we ensure an efficient use of the right technology at the right time.
Advances in information technology offer the potential of proving health system managers with a more ‘information rich’ environment on which to base decisions. Ultimately, this trend will help support a more integrated approach to care and should improve efficiency. We’re not there yet of course – but we have a better idea about where to focus policy effort. Genuine efficiency can support rather than stifle innovation. That’s what we need to promote.
Source: OECD Health Statistics Database (accessed 2013)
